
AONL COVID-19 Longitudinal Study Finds Top Challenges for Nurse Leaders
The American Organization for Nursing Leadership (AONL) and Joslin Marketing, Richmond, Va., partnered to conduct a longitudinal study on the impact of COVID-19 on nursing leadership in July 2020 and February 2021. The recent findings indicate changes to primary challenges and levels of support, with new findings on mental health and advocacy concerns. The February 2021 Longitudinal Study identifies critical changes that have occurred in health care since July 2020. This article features highlights from the February survey; the full report can be viewed at aonl.org/resources/nursing-leadership-covid-19-survey.
Since the initial survey, evidence has emerged indicating access to personal protective equipment (PPE) has improved while the challenge of mental health and staffing have worsened. As stated by one nurse leader: “We have seen nurses leaving the profession due to moral distress, burnout and fatigue. I believe if we can address the root cause of this problem, we will retain more nurses and begin to stabilize the numbers in the workforce.”
The February 2021 survey is part of an ongoing longitudinal study designed to track several areas over time. The initial survey was completed in July 16-26, 2020, with 1,824 leaders responding. Findings from the first survey were published in the December 2020 issue of Nurse Leader. Nearly one out of three respondents in the second survey recalled completing the initial survey. The second survey was sent to 23,515 nurse leaders and completed or partially completed by 2,471. The margin of error for the second survey was +/- 2.45% with a 99% confidence level.
Of the respondents from the February 2021 survey, 87% were either chief nursing officers (CNOs), chief nursing executives (CNEs), vice presidents, directors or managers. Overall, 34% of the respondents were directors, 32% managers and 17% CNOs or CNEs.
The majority of respondents came from acute care hospitals (52%) or health system facilities (14%). Only 4% came from long-term acute care or post-acute care facilities. Of all the respondents, 51% were urban, 29% suburban and 20% rural.
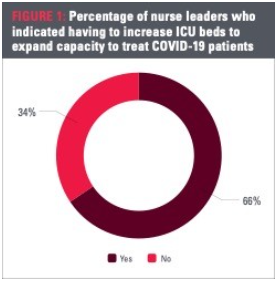
Increasing intensive care unit (ICU) beds is a direct indicator of surge. Similar to the percentage of nurses needed to treat COVID-19 patients, the percentage of ICU beds needed to expand capacity to treat patients increased by 12%, with a total of 66% of leaders reporting an increase in ICU beds. A variance emerged between CNOs and managers’ responses. Fifty-seven percent of CNOs reported an increase in ICU beds to accommodate patients, compared to 70% of managers. Of all respondents who reported having to increase ICU beds to expand capacity, 44% said they increased beds cumulatively over 6 months since the start of the pandemic.
Professional development
Respondents indicated the percentage of nurses that received professional development to perform additional or new competencies to expand capacity to treat COVID-19 patients. Half of all respondents said 81-100% of their nurses were trained, a 2% increase from July 2020.
In addition to how many nurses received professional training, nurse leaders were asked to identify the percentage of nurses actually utilized to treat COVID-19 patients. One third indicated 81-100% were needed, which was a significant 10% increase from the results in July 2020.
Top challenges then and now
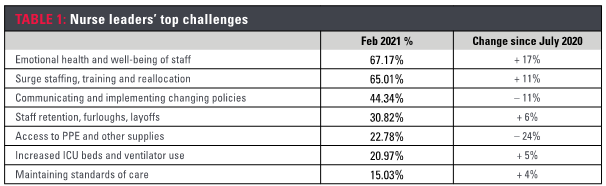
In the July 2020 survey we asked nurse leaders to identify their top three challenges:
- 54% selected communicating and implementing changing policies
- 53% selected surge staffing, training and reallocation
- 49% selected mental health and well-being of staff
- 46% selected access to PPE
In the February 2021 survey the attention narrowed to two major challenges:
- 67% selected mental health and well-being of staff
- 65% selected surge staffing, training and reallocation
- 44% selected communicating and implementing changing policies
- 31% selected staff retention, furloughs and layoffs
Significantly, the percentage of nurse leaders who selected access to PPE dropped by 24% since July 2020.

After respondents indicated their top three challenges, they were asked to rate how effectively they have been able to address those specific challenges. They were asked to rate on a 1-5 scale, with 5 being very well. The mean score for all challenges was 3.51, or between neutral and well. The lowest overall mean scores were 1) financial resource availability (2.84); 2) staff retention, furloughs and layoffs (2.92) and 3) health inequity and the impact of social determinants of health (2.97). For CNOs, the lowest score was staff retention, furloughs and layoffs. For directors and managers, the lowest score was indicated for financial resource availability.
For the February 2021 survey, respondents were asked to identify the biggest challenge they face today that they did not face six months ago. For this question, respondents selected only one challenge, opposed to the previous question where they selected the top three overall challenges. In the recent survey 35% of respondents named low morale and burnout as their number one challenge. This is followed by staffing shortages and vaccine administration at 16% and 10%, respectively. A gap between CNOs and managers is evident. Only 28% of CNOs selected low morale and burnout as a new challenge, compared to 43% of managers, for a 15% gap between the roles. This statistic is linked directly to managers’ overall emotional health and well-being. Similar to other questions, directors were in the middle at 34%.
For CNOs, staffing shortages were as critical as low morale and burnout. More than one-fifth of CNOs selected it as their top challenge. This was consistent with our interviews, where nurse leaders frequently expressed concern with staffing shortages due to a number of causes, including nurses leaving to care for their children, seeking higher pay and early retirement. Together staffing inconsistency and cost of staffing accounted for 12% of respondents’ selections.
Respondents were asked to provide open-ended details as to how they have adapted to the challenges, naming adaptations, behaviors, structures or innovations that have been beneficial.
Morale and burnout
Many tactics are being used to address burnout and low morale. The focus on engagement of staff, being present, creating a safe space for honest communication and listening to their concerns were the most frequent responses.
Staffing shortages
More than one out of four nurse leaders reported that their primary tool for addressing their staffing shortage was the use of travel and temporary nurses. Another 25% used monetary incentives and bonus pay to ensure staff availability.
Staffing retention
Unlike the other responses, nurse leaders provided a description of the problem versus the solution. They focused on turnover issues due to travelers, higher pay positions, low acuity environments and family safety concerns.
Future needs
In the initial survey, nurse leaders identified temporary advancements that would be the most needed to maintain beyond the COVID-19 crisis. At that time, 45% of respondents selected increased utilization of telehealth. While this remained the leading choice for the February 2021 survey, its significance decreased by 9%, with wider recognition of nurses’ contributions closing the gap. Together, these are the top advancements nurse leaders would like to maintain, with nearly two out of three nurse leaders selecting one or the other. Adoption of new staffing models and increased interdisciplinary collaboration were the next advancements to top the list. For CNOs, there was relatively equal emphasis for telehealth (33%), interdisciplinary collaboration (33%), and staffing models (31%).
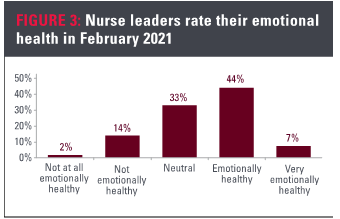
Measuring emotional health
For the February 2021 survey, nurse leaders rated their current emotional health on a 1-5 scale, with 1 being not at all emotionally healthy and 5 being very emotionally healthy.
- 16% selected not or not at all emotionally healthy
- 33% selected neutral
- 51% selected emotionally or very emotionally healthy
The most alarming statistic concerns managers. Managers lean towards emotional distress compared to their peers. One out of four managers indicated they are not or not at all emotionally healthy. Only 41% selected emotionally or very emotionally healthy, compared to 51% across all roles. In comparison, 65% of CNOs selected emotionally healthy or very emotionally healthy. Only 7% of CNOs reported being not or not at all emotionally healthy, 17% less than managers.
Staffing shortages Staffing shortages were one of the top challenges faced by nurse leaders at the time of the February survey. Staffing shortages, travel nurses and temporary staffing were mentioned in interviews with CNOs, directors, and managers as a constant concern. To provide quantitative data on an ongoing debate, nurse leaders were asked to indicate how likely their organization is to experience a shortage following the pandemic, rating between not at all likely and very likely. The mean score was 3.52, between neutral and likely. More than half of respondents selected likely or very likely, with 23% of all leaders selecting very likely. Notably, directors were most likely to expect a shortage; 25% selected very likely and 37% selected likely. Overall, only 4% said they are not at all likely to experience a staffing shortage.
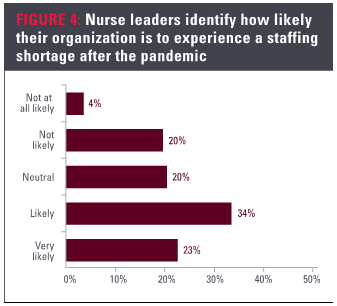
Respondents were asked to provide an open-ended response to the primary cause of their staffing shortage. Nearly one-quarter of respondents named burnout and fatigue as being the primary cause. Others said early retirements, travel nursing and nurses leaving the profession. In some cases, poor leadership was said to be the primary cause. One nurse leader noted, “Staffing was an issue prior to the pandemic. The pandemic has exacerbated the issue.”
Policy concerns
Another addition to the February 2021 survey was an advocacy question to determine the key areas for desired policy change. Validating the top challenge, burnout and behavioral health received 45% of the response. Following was grants and loan repayments for nurses and faculty, tailed by cost of travel and temporary nurses. These received 18% and 16%, respectively. Clinician childcare, transportation and housing support cumulatively received 9% of selections. Visa recapture was selected by less than 1% of nurse leaders.
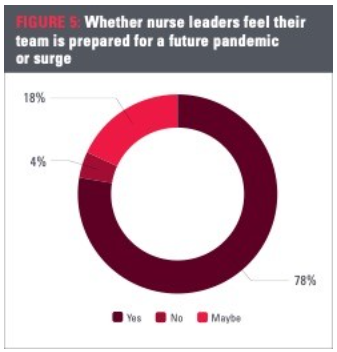
Preparation for the future
Since July 2020, confidence in preparedness has declined. In the initial survey, 87% of nurse leaders said their team was prepared for a future pandemic or surge. That number has dropped by 9% over the past six to seven months. After experiencing a rapid surge in the fall that continued throughout the winter, 78% of nurse leaders now say they feel their team is prepared for a future pandemic or surge. Overall, 18% said maybe, with over 4% saying no. When analyzing roles, the gap remains, with 84% of CNOs said they feel their team is prepared, while only 74% of managers indicated the same.
Looking ahead
At the end of the first longitudinal survey in July 2020, the total death count in the U.S. was under 130,000 and new cases were declining in the Tri-state region (New York, New Jersey and Connecticut), with the first wave just reaching Florida, Arizona and California. At that time, communicating and implementing changing policies and surge staffing, training and reallocation of staff were the top challenges nurse leaders faced, as well as access to PPE and other equipment. Fast forward six months and the story changed dramatically.
At the end of the second survey in February 2021, the death count in the U.S. exceeded 500,000. Access to PPE was far less of a concern, and emotional health and well-being skyrocketed as a problem, with over 67% of nurse leaders identifying it as a top challenge. As of February 2021, one-fourth of managers reported they were not or not at all emotionally healthy. Surge staffing, training and reallocation remained a challenge, having increased since July 2020.
Going forward, the acute problem facing health care is the emotional health and well-being of nurses. It is clear from this study that nurse managers are exposed to higher levels of stress and that the closer they are to the point of care, the greater the effect the crisis has on emotional health. Staffing shortages, as well as travel and temporary nursing models, must also be considered from an operations perspective and for future policy initiatives.
ABOUT THE AUTHORS
Daryl Joslin is principal and executive advisor at Joslin Marketing, Richmond, Va.
Hunter Joslin, MA, is associate principal and research analyst at Joslin Marketing, Richmond, Va.


