
AONL COVID-19 Yearlong Study Follows

The American Organization for Nursing Leadership (AONL) and Joslin Marketing partnered to conduct a longitudinal study on the impact of COVID-19 on nursing leadership. The study was launched as a series: July 2020, February 2021 and August 2021. The recent findings reveal changes to nurse leaders’ primary challenges and critical data concerning staffing shortages and nurse leader well-being. This article features highlights from the August 2021 survey; the full report can be viewed at aonl.org/resources/nursing-leadership-covid-19-survey.
The August 2021 survey, funded by the AONL Foundation, was the third and final part of a yearlong longitudinal study designed to track several areas over time. The first survey was completed July 16-26, 2020, with 1,824 nurse leader respondents. The second survey was completed at the midway point by 2,741 nurse leaders between February 8-18, 2021. The third survey, launched August 10-20, 2021, was completed or partially completed by 1,781 nurse leaders. The majority of respondents from the third survey identified as white/caucasian, over the age of 45, and from urban acute care hospitals. Eighty percent were either chief nursing officers, chief nursing executives (CNOs/CNEs), vice presidents, directors or managers. By role, 29% were directors, 25% managers, and 20% CNOs/CNEs. Fifty-two percent of respondents came from acute care hospitals and 16% from health system facilities. Only 4% came from long-term acute care or post-acute care facilities (skilled nursing, inpatient rehabilitation, etc.). Half of respondents identified as urban, 33% suburban and 17% rural.
Top challenges then and now
In July 2020, 54% of respondents said communicating and implementing changing policies was a top challenge. Over the course of one year this has improved steadily. Today, only 34% of respondents selected it as a top challenge, a 37% decrease. Similarly, the challenge of personal protective equipment (PPE) and other supplies dropped from 46% to 14%, a 70% decrease. Conversely, the emotional health and well-being of staff has become an ever greater problem. In July 2020, 50% of nurse leaders selected it as a top challenge. In just the past year, that number has increased with 75% of respondents selecting it as a top challenge, a 50% increase. Also alarming is staff retention, furloughs and layoffs. In July 2020, 24% of nurse leaders identified it as a challenge. Today, that number has increased by 96%, with 47% of nurse leaders now selecting it as a top challenge (Figure 1).
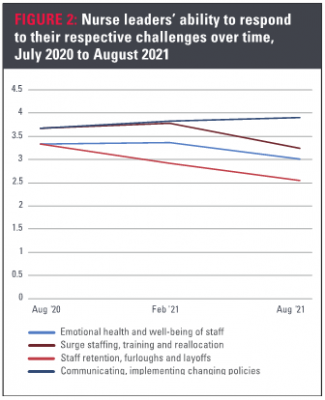
Responding to challenges then and now
For all of our surveys, respondents were asked to rate how effectively they have been able to address their respective top challenges. They were asked to rate on a 1-5 scale, with 5 being very well. In August 2021, the mean score for all challenges was 3.28, compared to 3.51 in July 2020. When analyzing the top challenges, we can see where nurse leaders are struggling to respond and where they are improving. In communicating and implementing changing policies, nurse leaders are making headway. Staff retention, furloughs and layoffs; emotional health and well-being of staff; and surge staffing, training and reallocation, however, have continued to provide nurse leaders with difficulty as their ability to respond to these challenges worsens. Since July 2020, the ability to respond to staff retention, furloughs and layoffs has declined most significantly, with the nurse leader’s ability to respond to this challenge dropping by 24% over the course of one year (Figure 2).
Staffing shortages spike
For the February and August 2021 surveys, we asked respondents to identify the greatest challenge they face today that they did not face six to eight months ago. The goal was to determine emerging challenges. As of August, 38% of respondents named staffing shortages as the biggest new challenge—a staggering 137% increase since February. The growing staffing shortage does not come as a surprise. A global staffing shortage is occurring across a range of industries as organizations struggle to fill vacant roles and adapt to the changing economy—one that is being driven increasingly by employees’ needs.
Following staffing shortages was low morale and burnout, which was the top new challenge in February. Concerning health care roles, a gap between CNOs/CNEs and managers is evident. A higher percentage of managers (37%) selected low morale and burnout, compared to CNOs/CNEs (22%). Conversely, 45% of CNOs/CNEs selected staffing shortages as the biggest new challenge, compared to 37% of managers. Notably, vaccine concerns—vaccine administration and vaccine hesitancy—account for 10% of the selection.
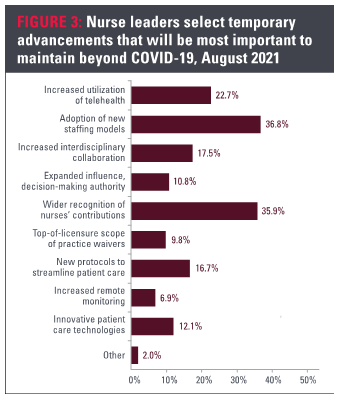
New staffing models, nurse recognition make gains
Since the initial survey, we have asked nurse leaders to identify the top two temporary advancements that should be maintained beyond COVID-19. In July 2020 at the onset of the pandemic, 45% of respondents selected increased utilization of telehealth. Since then, telehealth’s significance has declined by 51%. Today it accounts for 23% of respondents’ selection. Similarly, increased interdisciplinary collaboration has declined since July 2020. Previously, it accounted for 26% of the selection, compared to 17% today.
While these drop, new innovations emerge as frontrunners. Adoption of new staffing models and wider recognition of nurses’ contributions have both increased significantly since last summer. Previously, adoption of new staffing models received 28% of the selection. This has increased by 38% over one year. More significantly, the need for wider recognition of nurses’ contributions has increased by 48% over the same time period. Previously, recognition received 24% of the selection; now it accounts for 36% (Figure 3).
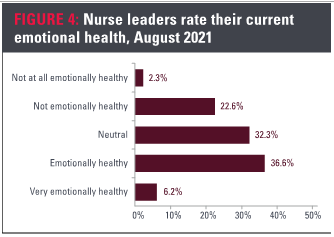
Emotional health and well-being worsens
The most alarming statistic concerns the emotional health of nurse leaders, which is dropping at a critical rate. As of August 2021, 25% of nurse leaders say they are not emotionally healthy. Managers, specifically, tend toward emotional distress. In February 2021, 24% of nurse managers indicated they were not or not at all emotionally healthy. That number has risen by 50%, with 36% now reporting being not or not at all emotionally healthy. While scores for emotional health are better among CNOs, CNEs and directors, these groups also are trending toward lower levels of emotional health. In February, 7% of CNOs and CNEs selected not or not at all emotionally healthy. That number has increased by 143% in just six months, to 17% in August. Similarly, 26% of directors now report not being emotionally healthy, a 73% increase over the same time period. (Figure 4)
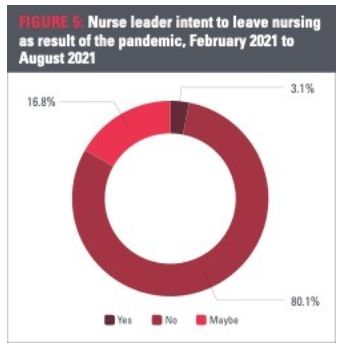
Intent to leave nursing grows
The February 2021 survey findings showed 90% of nurse leaders said they would not leave nursing due to COVID-19. However, while nurses have demonstrated a superhuman ability to cope in the face of crisis, they are human. Faced with new challenges, growing staffing shortages and declining emotional health, data now shows that intent to leave is beginning to grow.
The August 2021 data reveals a negative trend with 80% of nurse leaders saying they intend to stay in nursing, down 10 percentage points from six months earlier. In August, nearly 17% of nurse leaders said they are considering leaving, a 116% increase since February 2021; and 3% of nurse leaders say they plan to leave, a 90% increase over the same period of time.
Of those who said they intend to leave, 53% said they were not sure when, 22% said within one year, 14% within the next six months, and 5% within one month. Six percent said they would leave when the pandemic is over (Figure 5).
Post-pandemic staffing shortages projected
To understand the full extent of the staffing shortage problem and future projections, we asked nurse leaders to indicate how likely their organization is to experience a staffing shortage following the pandemic. Respondents were asked to rate between not at all likely and very likely. The findings were some of the most dramatic since February 2021. The mean score previously was 3.52, between neutral and likely. As of August 2021, the mean score jumped 26% to 4.44, between likely and very likely. Most significant, however, was the increase in respondents who said a staffing shortage is very likely. This number increased by 165%, jumping from 23% to 60% over six months. Overall, 90% of nurse leaders expect a post-pandemic staffing shortage.
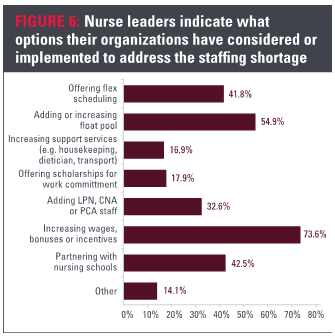
Addressing staff shortages
We asked nurse leaders to indicate what options their organization has considered or implemented to address the staffing shortage. Seventy-six percent of respondents selected increased wages, bonuses or incentives. This was followed by 56% adding or increasing float pools, 43% partnering with nursing schools and 42% offering flex scheduling. Another 34% said they have considered or implemented adding licensed practical nurses, certified nursing assistants or patient care assistant staff. Notably, 17% also said their organization has considered or implemented increasing support services such as housekeeping, dietician or transport (Figure 6).
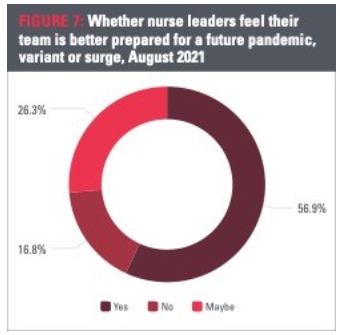
Confidence declines
Throughout the longitudinal study, we asked nurse leaders if they feel their team is better prepared for a future surge, variant or pandemic. The first survey from summer 2020 indicated the highest level of confidence in future pandemic response as 87% of nurse leaders said they felt their team was better prepared. This score has dropped by 34% within the last year to a 57% confidence level. Overall, 26% of nurse leaders now say maybe their team is better prepared, and nearly 17% indicated they are not better prepared (Figure 7).
Workforce investment needed
The yearlong longitudinal study has highlighted staffing shortages and retention as a growing concern, with 90% of nurse leaders anticipating a shortage after the pandemic. Hospitals and health systems join a global staffing shortage as they struggle to fill vacancies and adapt to a new economy. Emotional health is declining, with 25% of nurse leaders reporting being not emotionally healthy. Nurse leaders’ intent to leave has increased by 123% in six months, while confidence in preparedness for a future surge, variant or pandemic has declined by 34% in one year.
Hospitals, health systems and organizations have implemented a number of strategies to address these challenges, such as increased pay and bonuses. Following the mass vaccine roll-out and drop in new COVID infections during spring 2021, health care began to see a glimmer of hope. We hoped many of the alarming workforce trends would have plateaued by the time AONL and the AONL Foundation launched its summer survey. However, in the midst of yet another surge, it is clear health care workers are struggling and challenges are increasing. From increasing support services for health care workers, to recruiting and retention, addressing these issues requires an investment in the health care workforce.
About the Authors
Daryl Joslin is principal and executive advisor at Joslin Marketing, Richmond, Va.
Hunter Joslin, MA, is associate principal and research analyst at Joslin Marketing, Richmond, Va.

